The Truth About Semaglutide
An Interview with Dr. Mary
What is Semaglutide?
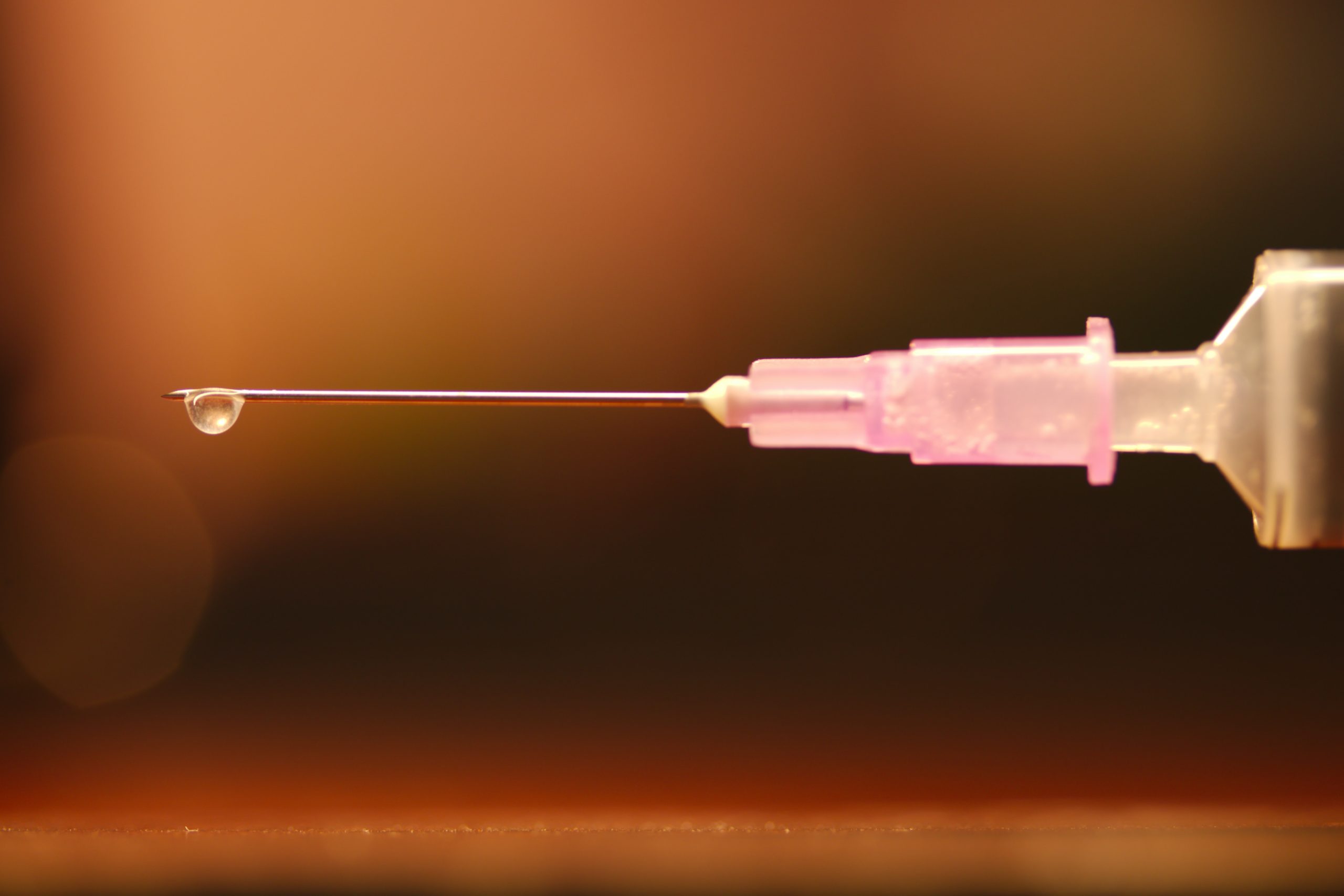
Dr Mary: This is the anti-diabetes and anti-obesity drug you’ve heard about in the news. It’s an injectable medication that has been approved for the treatment of type 2 diabetes since 2017 but is getting attention now because of results from a recent clinical trial that showed that participants lost, on average, 17% of their body weight without significant changes to what they were eating. The medication is administered in an injectable pen that can be stored in the refridgerator or at room temperature, though it’s best to store it in the refrigerator to avoid the risk for bacterial growth.
Semaglutide is a glucagon like peptide-1 glp-1 (a specific amino acid chain) that acts as a GLP1 agonist, which lowers blood sugar levesla and makes you feel fuller for longer. Semaglutide is the generic name, and it’s sold under the brand names Ozempic (approved in 2017 for diabetes), Wegovy (approved in 2021 for obesity), and Rybelsus (approved in 2019 for oral use) all made by Novo Nordisk. After these recent promising clinical trials, it’s now being used widely, not just for adults with type 2 diabetes and obesity but for long-term weight management.
How does it work?
Dr Mary: It works in a few different ways. Firstly, by slowing gastric emptying. This makes you feel like you’re getting full faster and staying full for longer. It’s also impacting the satiety center in the brain to make you feel more satiated. The idea is that you’re able to listen to your body and stop eating when you feel full.
It also helps reduce blood sugar by slowing down glucagon production. Reduced blood sugar, of course, helps with insulin resistance, which is also called pre-diabetes. This is shown with improved hemoglobin A1C markers in the blood. It’s worth noting that this drug manages to lower blood sugar without causing hypoglycemia, which is a major positive as hypoglycemic episodes can be very dangerous, especially for patients with type 2 diabetes.
Through lowering blood sugar levels, semgalutide reduces symptoms of high blood sugar that are associated with diabetes, including frequent urination, thirst, diabetic retinopathy, nerve damage, vision changes and cardiovascular risk. These symptoms arise becuase of microvasulcar damage from the high sugar in the blood, which prevents oxygen exchange at the microvasculature. By reducing blood sugar levels, semaglutide addresses these symptoms at the root cause.
It’s likely so impactful because it’s working at the levels of both the gut and the brain. Feeling physically full and satiated or satisfied are two different things, and this seems to address both.
What are the risks or common side effects?
Dr Mary: Potential side effects are nausea, abdominal pain, distention, reflux, and bloating. The dosing schedule is important. Like many other drugs, it’s imperative to titrate (go up on dose) slowly. Your doctor should start you on a very low dose and gradually increase it over time as you tolerate the drug. Ex: if you are vomiting, you are not tolerating the dose.
There is also a concern about tolerance, meaning that patients may become more and more tolerant of the drug over time, leading to a perpetual need to increase the dose.
There’s also some fear that long-term use could cause thyroid cancer. We don’t have studies that follow the drug years out, over the long term, to assess this type of risk.
I do think we can feel slightly safer about this drug because it’s a peptide. Peptides are chains of amino acids that build into a protein. The beauty of peptides is that usually, it’s hard to overshoot, meaning the body will not allow you to overdose on a peptide. Peptides are a natural part of your body that the body knows how to regulate intuitively. The FDA has ruled that if the peptide is longer than 40 amino acids, it is now considered a “drug.”
If a patient has failed a trial of metformin or is still not losing weight with other diabetic agents, or if you are trying to avoid the increased heart rate and other risks associated with appetite suppressants, I believe this is a good option.
So it seems effective and relatively safe. Is there a catch?
Dr Mary: It’s very expensive, and the companies are happy for it to be a “forever drug.” This means that once you stop it, if you haven’t changed your lifestyle and reduced the toxins you’ve been exposed to, like seed oils and processed food, studies show patients gain the weight right back.
Can you elaborate? What is your opinion about the use of semaglutide?
Dr Mary: Some of the reasons I’m having trouble with this are the lack of long-term studies, the expense, and the lack of education about how to eat clean real food moving away from toxins.
We’ve seen this before. Drug companies are luring people in with special prices and coupons to get started, the patients see results on the drug, and then prices historically have gone up after the person has been using the medicine for a while. Since semaglutide was first developed for treating type 2 diabetes, many insurances still will not cover the prescription, brand name, or generic for weight loss. So if the patient doesn’t qualify with type 2 diabetes, they may end up with a pretty substantial added monthly expense.
Of course, anything that addresses weight loss and lowering blood sugar levels will get my attention because I recognize that obesity and insulin resistance is at the root of almost all health conditions I see. I’m all about getting to the root cause, and often losing weight allows the body to restore optimal function and get back into balance. From that perspective, this is an exciting drug if it means getting the weight off people who have tried and failed previously with metformin and other efforts at weight loss.
But there’s a big “but.” If you don’t teach them how to change their lifestyle and diet while they’re on the drug, they will become entirely dependent on it, meaning if they stop taking it, the weight will return. I think it’s dangerous to depend on a drug for weight loss without simultaneously addressing the diet, lifestyle, emotional relationship to food, and all the other aspects that go into long-term, sustainable drug-free weight management.
Suppose we can assure there is little to no short-term or long-term risk of developing cancer, and you have a patient who will need to be on a “forever drug” to manage their weight and/or diabetes. In that case, I think this is a much better option than insulin, for example.
Despite the potential risks, I am still cautiously recommending it because I feel that the long-term benefit of helping a patient lose weight which will help get them off all their other medications, is greater than the potential risk.
I’m also recommending only the short-term use of this drug, using it temporarily as a bridge. I am, generally speaking, not in the game of long-term prescription drug use, but I can recognize when a medication may be effective in the short term to help a patient get over the hump to be able to make the long-term changes they need to make.
Do you use semaglutide with your patients?
Dr Mary: Yes. But to be clear, if I don’t teach you how to eat correctly while you’re on the drug, you will never get off it. So in my program, you may choose to try semaglutide for a period of time. Still, at the same time, you’re working with our coach and taking all of my other recommendations to integrate fundamental habits that will keep the weight off after you’re off the medication. I’m not okay with putting you on something to keep you on that forever.
(Find out more about Dr. Mary’s Optimal Wellness practice here.)
(Find out more about The Remedy Room’s weight loss coaching here.)
What do you feel people need to know that maybe they’re not reading about or hearing from other doctors?
Dr Mary: I think the potential risk for thyroid cancer is important and shouldn’t be brushed over. If you have a family history of medullary thyroid carcinoma, kidney problems, multiple endocrine neoplasia type 2 (tumors in your glands), or other risk factors, the drug isn’t a great option for you.
We need to be honest about the significant lack of long-term studies for semaglutide. While many things about how the drug works make the safety profile extremely promising, we simply don’t have the long-term clinical studies to make specific safety claims.
People need to know that the drug companies are marketing this drug similarly to how credit cards are marketed. These attractive, affordable initial offers lure people in to sign up. Then when the initial period is over, patients end up hooked and responsible for large out-of-pocket payments.
I want people to know that losing weight is at the root cause of so many of their symptoms of “dis-ease” and that they don’t need this drug to lose weight. With any combination of fasting, high-fat diets, the right supplements, and a great coach, we see patients in our clinic lose weight every day, and they almost all say that it was far more accessible than they had imagined.
We also need to treat this drug like other weight loss blockbusters from the past, like surgeries and appetite suppressants. The standard is that you’ve got twelve weeks to implement diet and exercise to improve weight for the long term once you come off the drug or heal from the surgery. The number of weeks might vary, but we need to keep that same mindset that this is a temporary bridge. We should also be looking for long-term safety studies and newer variations that might be even more effective. For example, tirzepatid, made by Elli Lilly under the name brand Mounjaro, is a promising next iteration of the semaglutide peptide, that stimulates two satiety hormone receptors instead of just one. Mounjaro is also contraindicated in patients with a personal or family history of MTC (medullary thyroid carcinoma) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN).
To summarize, I would say let’s proceed cautiously with semaglutide and use it as a temporary bridge to teach you the fasting and other lifestyle changes so that you can be empowered to come off the drug and keep the weight off for the long haul.
Learn more about Dr. Mary and The Remedy Room HERE.
If you’re interested in learning more or working with Dr. Mary personally in her Optimal Wellness Program, you can find more information HERE and book an initial consultation.
People Also Ask
What does semaglutide do to your body?
Semaglutide is a prescription drug used to treat type 2 diabetes. It is a glucagon-like peptide-1 (GLP-1) receptor agonist, which means it works by stimulating the body to produce more insulin when levels of glucose in the blood are high. It also helps to reduce the amount of glucose that is absorbed from the gut and decreases appetite, helping to control weight. Semaglutide helps to lower blood sugar levels and improve glucose control, reducing the risk of serious diabetes-related complications such as heart disease, stroke, and kidney damage. Additionally, semaglutide may also help reduce the risk of cardiovascular events such as heart attack and stroke, by reducing microvascular damage from high sugars. It is important to note that semaglutide should be used as part of a well-balanced diet and exercise program in order to achieve optimal results.
Is semaglutide worth it for weight loss?
Research suggests that semaglutide can be an effective tool for weight loss. In a study of overweight and obese participants, those who took semaglutide lost an average of 15% of their body weight compared to just 2.4% for placebo participants. Additionally, these participants showed improved blood pressure, cholesterol, and blood sugar levels as a result of their weight loss.
In comparison to other weight loss medications, semaglutide appears to be more effective and have less risks and side effects. A study compared the effects of semaglutide to liraglutide on weight loss in overweight and obese participants. Results showed that those taking semaglutide lost an average of 15% of their body weight compared to an average of 6% for liraglutide users.
Overall, semaglutide is promising for weight loss and may be an effective option for those looking to lose weight. However, it is important to speak with your doctor before taking any medication to ensure it is right for you. It it also important to note that there are risks associated with taking the medication if you have a history of thyroid cancer or other risk factors and that going on this drug should be treated as a bridge to help you lose the weight while you learn diet and lifestyle changes for long term sustainable success.
How fast is weight loss on semaglutide?
Studies have shown that those taking semaglutide lost an average of 14.9% of their body weight over a period of 68 weeks. Semaglutide is designed to help individuals achieve their weight loss goals over the long-term by making it easier to reduce caloric intake and increasing satiety. In addition, semaglutide can reduce cravings for unhealthy foods and increase energy levels, creating an overall healthier lifestyle. If you are looking for a safe and effective way to lose weight, semaglutide may be a good option for you, as long as you are also committed to making the diet and lifestyle changes necessary to eventually come off the medication.
How much weight can you lose with semaglutide?
Semaglutide is a medication used to treat obesity and has been found to be an effective weight loss aid. It works by activating the body’s natural processes that inhibit hunger and promote satiety. Studies have found that people taking semaglutide will lose an average of 15% of their body weight in 68 weeks, with some individuals losing even more than that. It should be noted, however, that semaglutide is only effective when combined with proper diet and exercise. Eating healthy and exercising regularly will help to maximize the benefits of this medication and improve overall health.